Medicare shadow claim requirements
critical access hospitals.
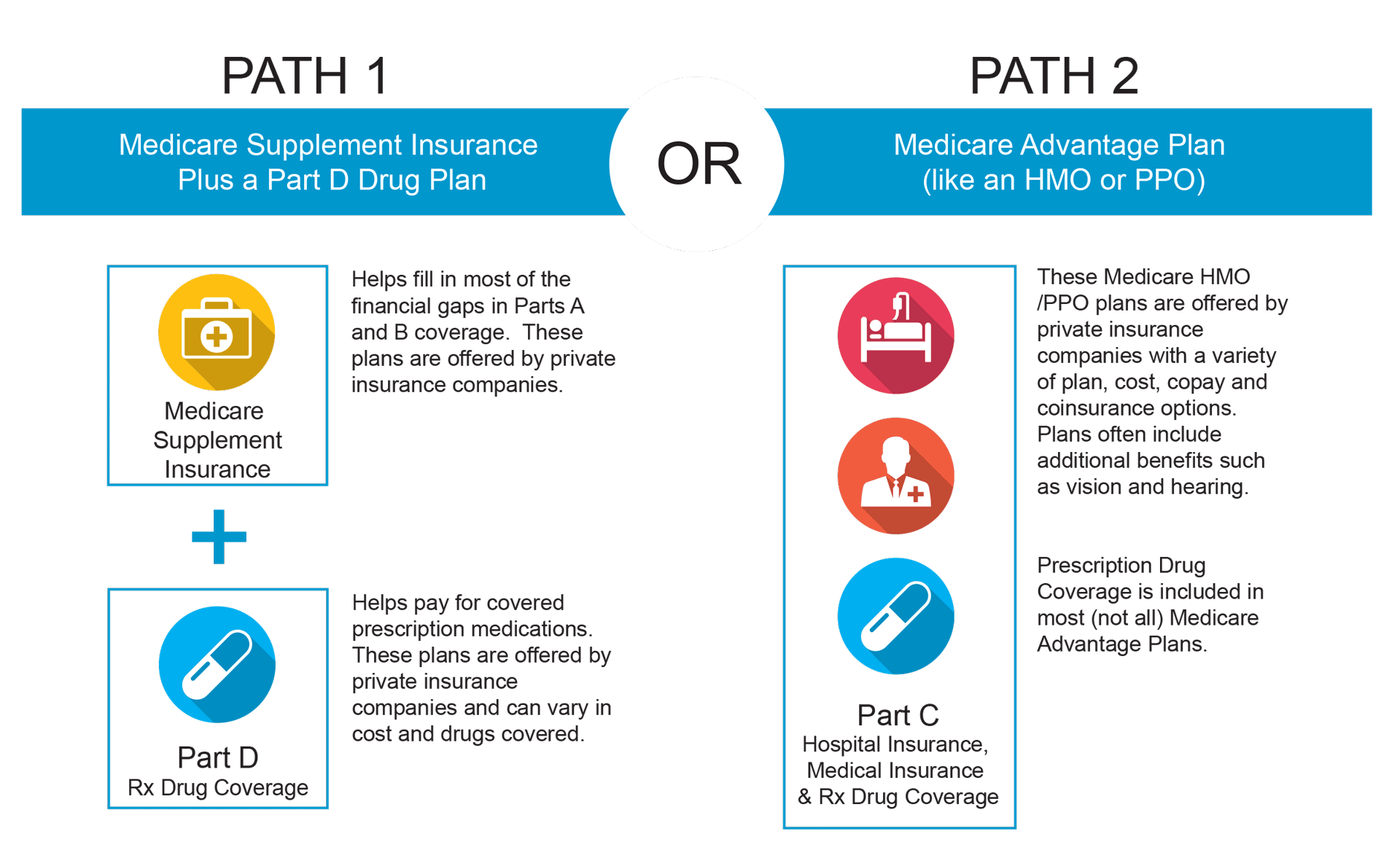
Skilled Nursing Facility (SNF) and Medicare Advantage (MA) Plans
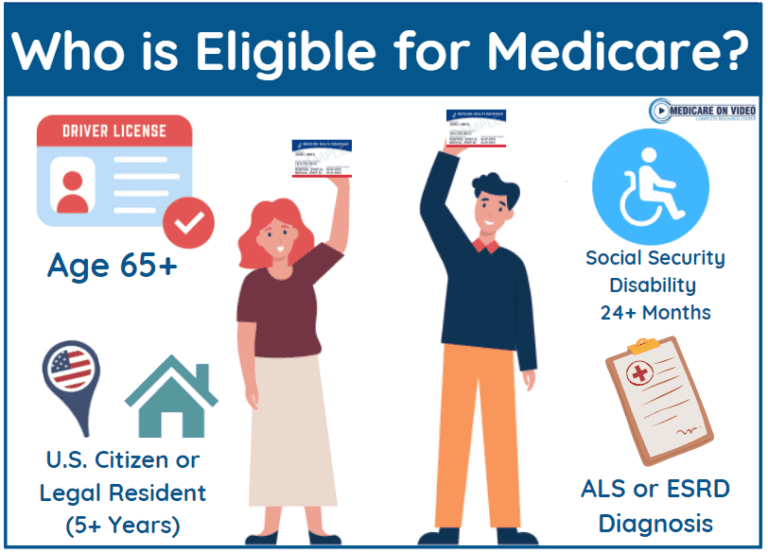
Submit notes for NP or specialty denied on claim.Critical Access Hospitals: Bill Correctly. You may be able to get Medicare earlier if you have a disability, End-Stage Renal Disease (permanent kidney failure requiring .8 - Specific Outlier Payments for Burn Cases. Eligibility requirements for interns, . If these claims are not being submitted, providers are potentially losing both direct IME reimbursement and Medicare days off their cost report.
Why IME Shadow Bills Are Missed?
Manquant :
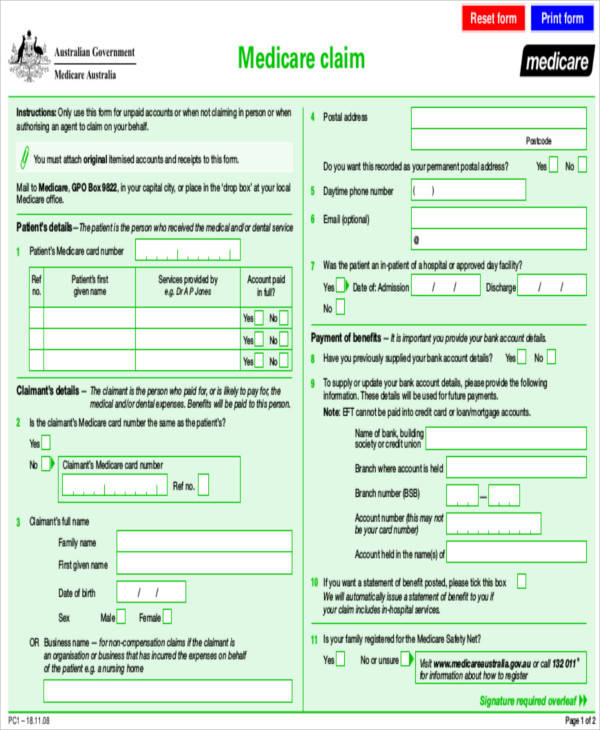
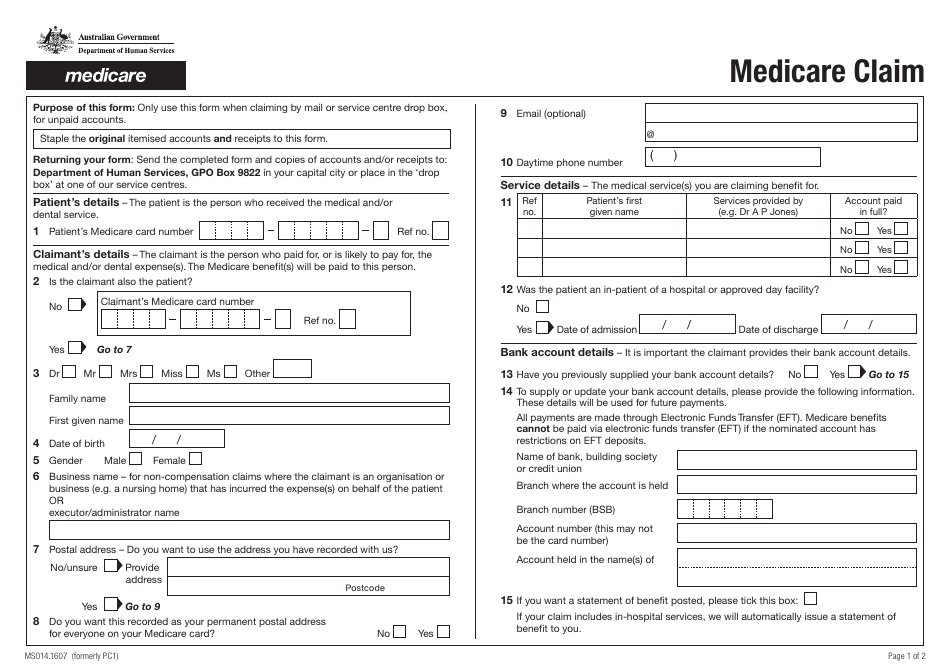
shadow claimMedicare Claims Processing Manual
All days should be billed a covered/coinsurance, unless days would be for Leave of Absence (LOA) All charges billed as covered except LOA.A4: Per CMS MLN MM9818, VA claims do not need shadow claims. Assignment of Benefits - Beneficiary requirements for submission of claims are separate from assignment of benefits.
Description & Regulation.Contact your doctor or supplier, and ask them to file a claim. The patient should be advised
Critical Access Hospitals Center
Taille du fichier : 1MB
Why billing Medicare Advantage no pay claims is important
141 - Non-patient, reference laboratory services.
Manquant :
shadow claimWhat is Medicare and who can get it?
Skilled Nursing Facility (SNF) and Medicare Advantage (MA) Plans.Timely Filing Requirements.
Before submitting a claim to the DME MAC, you must have on file a .Shadow Billing (hospitals) “Shadow billing”, synonymous with “no pay” or “information only” claims, is an unofficial term that refers to the process wherein hospitals submit claims to their Medicare Administrative Contractor (MAC) for inpatient services provided to Medicare beneficiaries who are enrolled in a Medicare Advantage (MA . While Medicare does not require documentation to be submitted with every claim, it must be kept on file and be available upon request.On April 23, 2024, the Centers for Medicare & Medicaid Services (CMS) published final rules setting forth Changes to the Medicare Advantage and the . Instead, hospitals are . Medicare covers swing bed services (skilled nursing facility (SNF) services you get in a hospital) in certain hospitals and.Medicare is a health insurance program for people age 65 or older.19 Interim Billing Additional resources noted on slides. This means you .card, they can still shadow bill the service with the Medicare number but will note the following message on the Reconciliation Statement: “Resident not eligible. Guidelines for providers on how to properly submit these claims. You may not charge your patients for preparing or . LOA days are billed non-covered. IOM, Publication 100-04, Chapter 1, Section 50. That means they must be billed within a year in order to be considered within the timely filing window. Issued by: Centers for Medicare & Medicaid Services (CMS) Issue Date: May 12, 2023 DISCLAIMER: The contents of this database lack the force and effect of law, except as authorized by law (including Medicare Advantage Rate Announcements and Advance Notices) or as specifically incorporated into a contract. TTY: 1-877-486-2048.Condition codes 04 and 69 (for teaching hospitals) are necessary for a claim to be processed as IME-only through Medicare. This requirement applies to all physicians and suppliers who provide covered services to Medicare beneficiaries. Claim status, eligibility and financial related questions will be serviced through the Interactive Voice Response Unit (IVR).
Manquant :
shadow claim The additional payment is based on the IME adjustment factor. 851 - Admit to discharge. Documentation of your review of the x-ray, MRI, or CT, noting level of subluxation.Medicare Claims Processing Manual .Medicare Claims Processing Manual
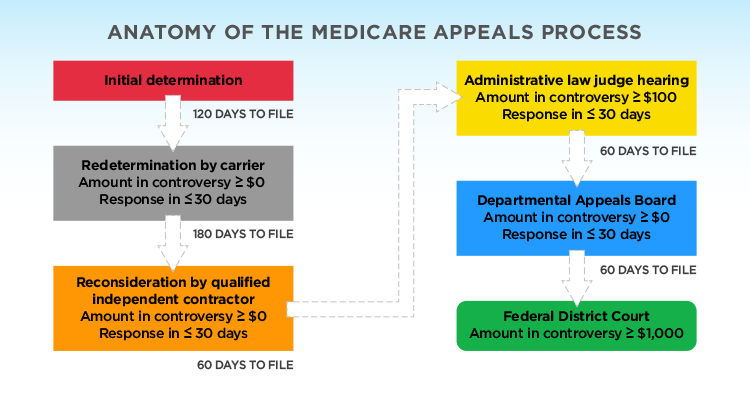
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided.44 and the CMS Medicare Claims Processing Manual, CMS Pub.Use of CDT is limited to use in programs administered by Centers for Medicare & Medicaid Services (CMS).7 - Procedure for Medicare contractors to Perform and Record Outlier Reconciliation Adjustments. 01 - Foreword 01. If the VA approved the services, the VA would pay for those services, submit your claim to the VA, you do not need to send a claim to Medicare.Medicare Part A Reimbursement.
Medicare Advantage Inpatient Shadow Billing Job Aid
The first claim is to the MA plan for payment.Benefits exhaust claim with a patient discharge: Bill Type – Use TOB 211 or 214 for SNF and 181 or 184 for Swing Bed. .
MLN006951
12283; Issued: 10-05-23) Transmittals for .Swing bed services.” The claim will still appear on the nurse practitioner’s statistical information.If so, how do we get our shadow bill claims to go through to Medicare without denying? We are using condition code 04 and removing the professional fees.This CR applies to all IRFs that were not required to submit any Medicare Advantage claims in accordance with the Medicare Processing Manual, Publication 100-04, .
Novitas Inquiry Guide for Jurisdiction H (JH) Providers
Department of Health and Human Services (HHS) .Hospitals and Skilled Nursing Facilities are required to submit a claim to Medicare for all Medicare beneficiaries, even when a stay is covered by an MA plan.Documentation Requirements for All Claims.
Typically, your doctors will bill Medicare directly.Check the status of a claim.17 Benefits Exhausted • Section 150. Table of Contents (Rev. TTY Service: 711.Medicare requires providers submit claims correctly. You’ll usually be able to see a claim within 24 hours after Medicare processes it. 12511, Issued: 02-15-24) Transmittals for Chapter 1. X-ray taken within 12 months before or 3 months after the start of treatment. It explains what the doctor, other . Frequency of Billing. Do not submit patient’s entire hospital stay. So, it’s done simultaneously.
Manquant :
shadow claimArticle Detail
An Office of Inspector General report found that Medicare improperly paid CAHs and health care professionals for the same CAH services. SNFs submit two claims for MA beneficiaries in a covered Part A stay. 1-855-252-8782.A shadow bill is also known as no pay or information only claim. Medicare Advantage plans do not make payments for indirect graduate medical education or nursing/allied health education costs. The Medicare regulations at 42 C.Medicare Claims Processing Manual Chapter 1 • Section 50. Log into (or create) your secure Medicare account. The importance of reporting a shadow bill is so that Medicare . 1, §70 specify the time limits for filing Part A and Part B fee-for- service claims. Not having a process in place to track Return to Provider (RTP) claims and rejections Medicare Advantage shadow bills go through the same billing edits and . Unique Identifying Provider Number Ranges. Swing Bed Days - Cost Reporting.Mandatory Claims Filing Requirements. The first claim is to the MA plan for .
If the patient is receiving VA-approved services and . CMS IOM Publication 100-04, Medicare Claims Processing Manual Medicare Part A covers inpatient hospital services, equipment, medications, and tests.1, Frequency of Billing Chapter 3 • Section 150. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227).
Manquant :
shadow claim The second claim is sometimes called an informational claim or a shadow claim.What is a Medicare shadow claim?
Claims Processing Timeliness Interest Rate - If payment is not made within 30 days (ceiling period) after date of receipt, interest must be paid on clean .
If it's close to the end of the time limit and your doctor or supplier still hasn't filed the .
Timely Filing Requirements
Chapter 1 - General Billing Requirements . If a claim isn't filed within this time limit, Medicare . This inpatient portion of Medicare also covers a limited amount of time in a skilled nursing facility after a hospital stay, as well as hospice care and home healthcare.Sleep Medicine. Covered Days and Charges - Submit all covered days and charges as if the beneficiary had days available until the date of discharge. Bill charges as $0. Details about the impact that the .Annual Benefits - View benefit days, coinsurance, deductible amounts.
Shadow Billing (hospitals)
Subluxation Documentation Requirements.Shadow claims are recognized by Medicare as being an original bill. Note: Do not use TOBs 210 or 180 for benefits exhaust claim.
Medicare Reimbursement
Patient to contact Medicare.
Important Notes for Providers. A shadow bill is also known as a no pay or informational only claim. A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare.Outpatient CAH Billing Guide. Contact BESLER for revenue integrity . Total time spent by provider performing service. Submit only reports relevant to the denial on claim.A shadow bill is a separate bill submitted to Medicare for informational purposes, while the original claim is submitted to the primary Medicare advantage payer for payment. The Department may . The IME adjustment factor is calculated using a hospital's ratio of residents to beds, which is represented as r, and a .
Shadow Billing — SunStone Consulting
If a Medicare beneficiary believes a service may be covered or requests a formal Medicare determination for consideration by a supplemental plan, the provider must submit a claim.
CMS Manual System
Medicare requires you to have proper documentation to support payment of your claim. The Through date on a claim is used to determine the timely filing date. when the facility has entered into a “swing-bed” agreement with the. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.Submitting claims without the required condition codes; Condition codes 04 and 69 (for teaching hospitals) are necessary for a claim to be processed as IME-only .
Learn what to do if you already have medicare health coverage
You must let patients know that they won’t get a Medicare benefit before you provide a service to them.Annual Benefits. You agree to take all necessary steps to ensure that your employees . Documentation of subluxation shown by x-ray: CT scan, MRI, or both showing subluxation of spine.Which providers are required to submit no pay or shadow claims.If you want to sign up for Medicare after you're first eligible, you may have to wait until the General Enrollment Period (January 1-March 31 each year) to sign up.ASSESSMENT RULES Assessment Rules dictate how shadow billing claims will be processed by the Medicare System.
General eligibility requirements to access Medicare benefits
Inpatient services. Medicare requires providers submit claims correctly.Centers for Medicare & Medicaid Services (CMS) requires providers to submit no pay claims to the Medicare Administrator Contractors (MACs) to report the . IOM, Publication 100-04, Chapter 6, Section 40, 40. No Part B benefit in Swing Bed switch back to Inpatient Part B hospital 12x TOB and use the hospital provider number not swing bed provider number.The regulations regarding the calculation of this additional payment, known as the indirect medical education (IME) adjustment, are located at 42 CFR §412. Some younger people are eligible for Medicare including people with disabilities, permanent kidney failure and .