Retained placenta postpartum

If not bleeding ensure the above steps are completed within 1 hour of diagnosis of retained placenta See Postpartum Haemorrhage guideline Complications of a Retained Placenta Uterine inversion Shock (hypovolemic) Postpartum hemorrhage Puerperal Sepsis Subinvolution Hysterectomy . This is when your uterus is overstretched from: Multiple pregnancies.8% of cases retained placenta [2–5]. Retained placenta: substantial amount of chorionic villi and products of conception retained in the uterus, typically causing . Initiate uterine massage as soon as excessive bleeding/uterine atony is identified. Manual removal of placenta increases the likelihood of bacterial contamination in the uterine cavity.Postpartum hemorrhage - diagnosis.The recommendation in this document thus supersedes the previous WHO recommendations on “intraumbilical vein injection of oxytocin for treatment of retained placenta” as published in the 2012 guideline, WHO recommendations for the prevention and treatment of postpartum haemorrhage. This is called a retained placenta. References (37) Cited by (6) European .WHO Guidelines for the Management of Postpartum Haemorrhage and Retained Placenta.To describe the association between quantity of blood loss, duration of the third stage of labour, retained placenta and other risk factors, and to describe the role of .Risk factors, early and late postpartum complications of retained placenta: A case control study - ScienceDirect. In group C, RPOC disappeared in approximately half of the cases at 100 days postpartum, and in 80% after 1 year postpartum. In these situations, more advanced examination .Retained placenta affects 0.It is one of the known abnormalities associated with ‘the four Ts’ (tone, tissue, trauma and thrombin) . Diagnosis is assisted by an ultrasound scan, with MRI indicated .Retained placenta complicates 2-3% of vaginal deliveries and is a known cause of postpartum hemorrhage. Treatment includes manual or operative placental extraction, . This may not be noticeable right away and the symptoms may only happen days, weeks, or even months after giving birth. When this happens, your .Normally, a woman’s placenta is expelled within 30 minutes of birth.Placenta, Retained - therapy.Emergency postpartum evaluation is warranted if the female rejects the cria or if obvious complications such as retained placenta, uterine prolapse, excessive vaginal bleeding, reluctance to stand, depression, poor appetite, postpartum colicky syndrome, or unexplained fever are present. Retained placenta (RP) affects 0. In the case of . An overdistended uterus also increases the risk for PPH.
BLS Treatment • Note amount of external bleeding • .In cases of missed retained placenta, the typical postpartum ailments and concerns can mask the symptoms.A placenta is deemed retained if not expelled within 30 min postpartum [6, 7].Placental remnants following birth are often heralded by secondary post-partum haemorrhage. Author: Midwifery Educator Classification: . To compare the effectiveness and side‐effects of routine antibiotic use for manual removal of placenta in . It is a known etiology for postpartum hemorrhage, because it impedes normal postpartum uterine involution. Etiologies include uterine atony, cervical or vaginal laceration, coagulopathy, and in 19. Having twins, triplets . It affects up to three percent of .Retained placenta is a life threatening emergency and a major cause of primary postpartum haemorrhage and maternal morbidity in the developing world.Women with retained placenta had a significantly higher rate of postpartum hemorrhage than women without retained placenta (11.Retained placenta occurs in around 1–3% of deliveries []. Can retained placenta affect milk supply? Many new mothers are concerned about low milk supply or a delay in milk production. But sometimes, the placenta does not come out after the birth.5–3% of all vaginal deliveries and is considered one of the major causes of primary and secondary postpartum hemorrhage (PPH), increasing maternal morbidity and mortality risk [1–5]. The only effective treatment is the surgical procedure of manual removal of placenta, which is costly, requires skilled staff, requires an operative environment and is unpleasant for women.


Objectives: To determine the socio-demographic .5% to 3% of women following delivery and is a major cause of maternal death caused by postpartum haemorrhage.
Retained placenta after vaginal birth
Postpartum Ultrasound
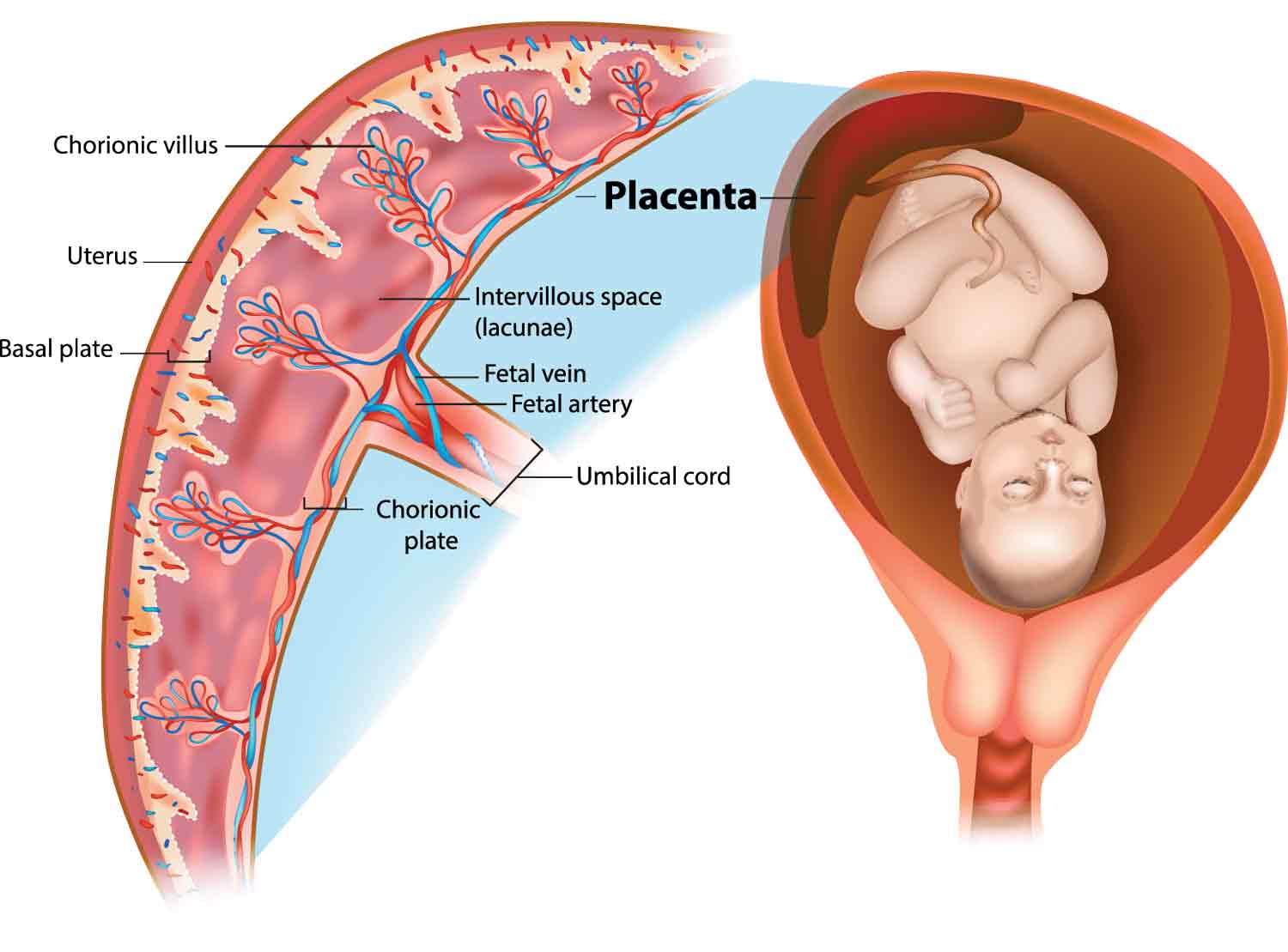
Those with placental problems like placenta accreta, placenta previa, placental abruption and retained placenta are at the highest risk of PPH. Normally, the placenta attaches to the top part of the uterus.The most common reason why the placenta is retained after childbirth is that placental villi adhere to the uterine myometrium without invading the decidua (placenta accreta), or the . Retained placenta can be caused by placenta accreta, increta, or percreta.06 Postpartum Hemorrhage – EMSAC . There are several complications of a retained placenta, including postpartum hemorrhage, which can lead to maternal death if not treated promptly.Retained placenta is a potentially life‐threatening condition because of its association with postpartum hemorrhage.What is retained placenta? Retained placenta occurs when your placenta isn't delivered within 30 minutes of vaginal childbirth. A retained placenta is usually . This condition is rare but dangerous. Retained placenta represents a cause of maternal morbidity and mortality affecting 0. This patient, a 34-year-old pregnant female, was admitted at 32 weeks of gestation for a case of preterm labor with preterm premature rupture of membranes and bacterial . Then it comes out of your body after the birth.Incidence of RP varies greatly around the world depending on the population studied [5, 6].A retained placenta is a rare complication affecting only about 2 to 3% of all deliveries that occurs when all or a portion of the placenta is left inside the uterus after .
Postpartum Bleeding and Retained Placenta: Care Instructions
Treatment includes manual or operative placental extraction, potentially increasing risks of . Treatment includes manual or operative placental extraction, potentially increasing risks of hemorrhage, infections, and prolonged hospital stays. Prevalence is higher in high- vs low-income countries (2.1% of maternal deaths, over two-thirds of which were classified as PPH [1]. This inability to contract causes severe bleeding of the blood vessels for about 24 hours and this .
Retained placenta and postpartum hemorrhage: time is not
The code is valid during the current fiscal year for the submission of HIPAA-covered transactions from October 01, 2023 through September 30, .Between September and October 2016 we searched PubMed using the following Mesh Terms: retained products, retained placenta, postpartum, and ultrasound.
Placenta Percreta occurs when the placenta grows all the way through the wall of the womb.
Postpartum hemorrhage is an obstetric emergency, accounting for 25% of all maternal fatalities.Retained placenta was observed in four patients in group M after the MROP, but the placenta disappeared more quickly than in group C (median; 1.Retained placenta “complicates 2-3% of vaginal deliveries and is a known cause of postpartum hemorrhage” . Despite the prevalence of this condition, there is limited guidance on its management. It also removes waste products. For most, infant led feeding is all that’s necessary to begin adequate milk production.retained placenta is diagnosed if the placenta is not delivered within 30 minutes following delivery of the fetus. Kordyws e : culling rates, dairy cows, postpartum diseases, retained place nta Introduction Retained placenta (RP) is defined as the retention of the fetal mem brane for > 24 h [10].On the list of postpartum complications, caused by the retained placenta bleeding is the most significant. Our results suggest that there is neither a safe time .Auteur : Kristen Sturt • Intravenous oxytocin alone is still the recommended uterotonic drug . However, no significant difference was found in the rate of postpartum blood transfusion between the women with a retained placenta and the women without a retained placenta (7.After a planned home birth turned hospital induction due to IUGR, she describes her early weeks postpartum, including latch issues with her tiny baby, trying to . The unpredictability of this . 1 Although a universal definition for retained placenta has yet to be established, most guidelines favor intervention to deliver the placenta if it has not spontaneously detached from the uterus within 30 min after delivery of the neonate, or .1% of maternal deaths, over two-thirds of which were classified as PPH []. Puerperium: the time after delivery until 6 weeks postpartum.
Placenta after birth: Symptoms of retained placenta
There are several complications of a retained placenta, including postpartum .Retained placenta after vaginal delivery is diagnosed when a placenta does not spontaneously deliver within a designated amount of time, variably defined as a .

We sought to evaluate risk factors for retained placenta, defined as more than 30 .When the placenta fails to separate spontaneously within a stipulated time or is delivered incompletely with a part of it still in utero, the diagnosis of retained placenta is almost certain [2,3,4].1 is a billable diagnosis code used to specify a medical diagnosis of retained portions of placenta and membranes, without hemorrhage.
I Wish I’d Known About the Risks of a Retained Placenta After Bir
If part or all of a placenta stays in the womb, it’s called a retained placenta. We report the case of a 32-year-old female, gravida 4 para 3, who was diagnosed with a retained placenta after delivering at .Retained placenta can be defined as lack of expulsion of the placenta within 30 minutes of birth of the neonate [ 1,2 ].Background: Retained placenta is associated with postpartum haemorrhage and can lead to significant maternal morbidity if untreated.
Retained Placenta Management
of postpartum dise ase s such as m e tritis and m astitis and is a culling hazard up to 60 DI M. Uterine Atony occurs when a woman’s . Postpartum hemorrhage (PPH) is the leading cause of maternal mortality worldwide: in 2003–2009, hemorrhage accounted for 27.The retained placenta is a risk factor for postpartum fever. We did not limit the search in time but we narrowed it down to English articles.3% of all vaginal deliveries and is one of the leading causes of postpartum hemorrhage worldwide.WHO guidelines for the management of postpartum haemorrhage and retained placenta.Retained placenta is caused by abnormal placental separation.
What Is a Retained Placenta?
Early postpartum hemorrhage is less than 24 hours after the delivery, and late postpartum hemorrhage means exceeding 24 hours after delivery.
Risk factors for retained placenta
RP is a serious While you can try to confirm with your OB/GYN .