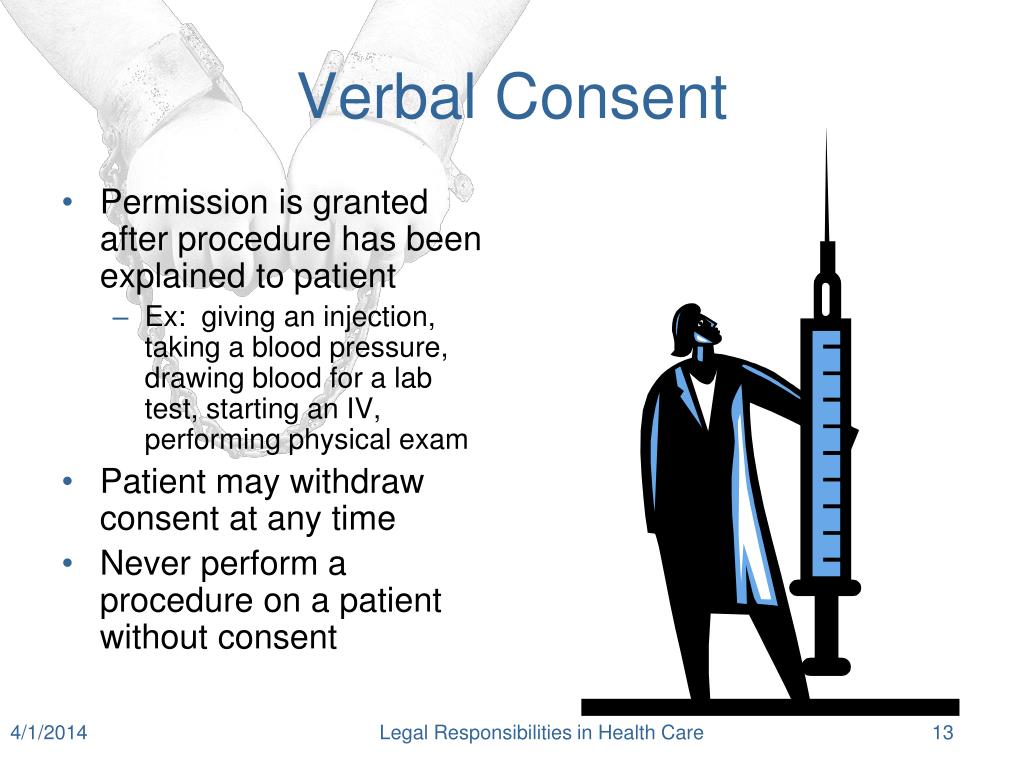
Verbal consent in health care
I give permission to [name of clinic or doctor’s office] to file for insurance benefits to pay for the .
in writing – for example, signing a consent form for surgery.
Evaluating models of consent in changing health research
Strong communication skills are essential to provide safe, quality, patient-centered care. To help you decide whether you want a treatment or procedure, your healthcare provider must give .govRecommandé pour vous en fonction de ce qui est populaire • Avis
Informed Consent in Healthcare: What It Is and Why It's Needed
Download PDF CME Course. Anyone who can .What is the purpose of informed consent? But in all cases, healthcare providers . Informed consent is an ongoing process of talking and asking questions between you, your doctor or other healthcare provider and, sometimes, your family/whānau.You have the right to make an informed choice about your health care.Although informed consent for clinical treatment has become a vital part of contemporary medical practice, it means different things in different contexts ( Figure 1 ), is variably practised and rarely achieves the theoretical ideal. A freeze response is an involuntary, . Implied Consent.The reality of informed consent: empirical studies on patient .The information appeared to have pertained to costs, pain, chances of success and duration of treatment. Reg 202/94 under the Pharmacy Act, the Health Care Consent Act (HCCA) and the Code of Ethics. One hundred (74.
Why Informed Consent Matters
Auteur : Heena Kakar, Ramandeep Singh Gambhir, Simarpreet Singh, Amarinder Kaur, Tarun Nanda
Informed Consent—We Can and Should Do Better
Auteur : Julia Lawton, Nina Hallowell, Claire Snowdon, Jane Norman, K Carruthers, Fiona Denison
Informed consent for clinical treatment
Manquant :
health care 1,2 The process of obtaining informed consent is an essential aspect of patient-centered care and remains central to patient safety.People need to give explicit verbal consent before receiving any vaccine, even if they gave written consent at previous vaccination encounters for the same vaccine. In this review, we focus on the clinical practice of informed consent.Babies, children and young people's experience of healthcare
There is an exception if the patient is in a licensed care facility. We first describe what we know about .What does ‘consent to treatment’ mean? Giving ‘consent to treatment’ for mental health means both that: You agree with a health professional about a treatment they've suggested for you. Informed consent to medical treatment is fundamental in both ethics and law. + Consent type.The ruling emphasizes the importance of patient autonomy, with consent to treatment now considered to be an indicator of the quality of patient care particularly with regard to safety, communication and respect for patients.
Judicial reviews and rulings by the Supreme Court mean that the need for “informed consent” is a legal . See further guidance in the NICE advice on .Informed consent has been a sticking point of the COVID-19 vaccine rollout, as older people in aged care were among the first to receive the vaccine if they agreed to the jab with informed consent.Getting Implied or Verbal Consent.Informed consent is a person’s decision, given voluntarily, to agree to a healthcare treatment, procedure or other intervention that is made: Following the provision of .Stated simply, informed consent in medical care is a process of communication between a clinician and a patient that results in the patient’s authorization or agreement to undergo .Similarly, if a consent platform can be set up as an extension of a pre-existing health care platform with assured accessibility and at low cost, this would count in favour of Meta Consent or Dynamic Consent Models. If a participatory process for determining normatively relevant categories of research can be established, Meta . So, God forbid, if I am ever sitting in a psychiatric unit again, here is what I will do to try and get implied or verbal consent: Inform the care team that I am her mother, she lives with me and I love her very much. 1–3 Guidance from the General Medical Council and Department of Health, 2,3 now reflects this ruling and brings the UK .
Verbal Consent Guidelines
The HHS regulations at 45 CFR part 46 for the protection of human subjects in research require that an investigator obtain the legally effective informed consent of the subject or the subject’s legally authorized representative, unless (1) the research is exempt under 45 CFR 46.This Permission To Bill Insurance letter is also available as a Word document (15 KB).79% of the respondents were told of alternative options available, 47. Implied consent is given daily in many healthcare situations but it is not sufficient for all types of cases. Consent is required to provide individual vaccines or a vaccine .1 Adhere to all relevant legislation and follow all national and local safeguarding policies and professional guidelines when implementing these recommendations and when planning and delivering healthcare services for all babies, children and young people, in any setting. Someone could also give non-verbal .

Audio recording and modeling of HHC patient-nurse encounters can allow the HHC team to enrich the documentation of patients’ information in electronic health records (EHRs) and facilitate the development of high-performing clinical decision support systems to identify HHC patients at risk of health care deterioration (eg, Alzheimer disease), . In some cases you can also give non-verbal consent, for example holding out your arm for . The medical provider must disclose information on the treatment, test, or . This does not involve treatments that involve placing an adult in hospital for the treatment of a mental disorder . As such, when minors seek abortion care, this may create a conflict between the value of confidentiality and the legal obligation to .Researchers must consider the setting and timeliness of the consent process.Consent may be communicated verbally or in writing, or may be inferred from the patient’s actions as further described in the section on consent type. At SVHM, consenting/re-consenting is usually undertaken in person with the Principal Investigator (PI), or Associate Investigator (AI) (if that person has HREC approval to obtain consent) to ensure that the participant has .101(b); (2) the IRB finds and documents that informed consent can be waived .However, health policy and guidance in NSW suggests there may be wider misinterpretation of the common law Duty of Care within the context of DMC and consent. The Joint Commission’s .
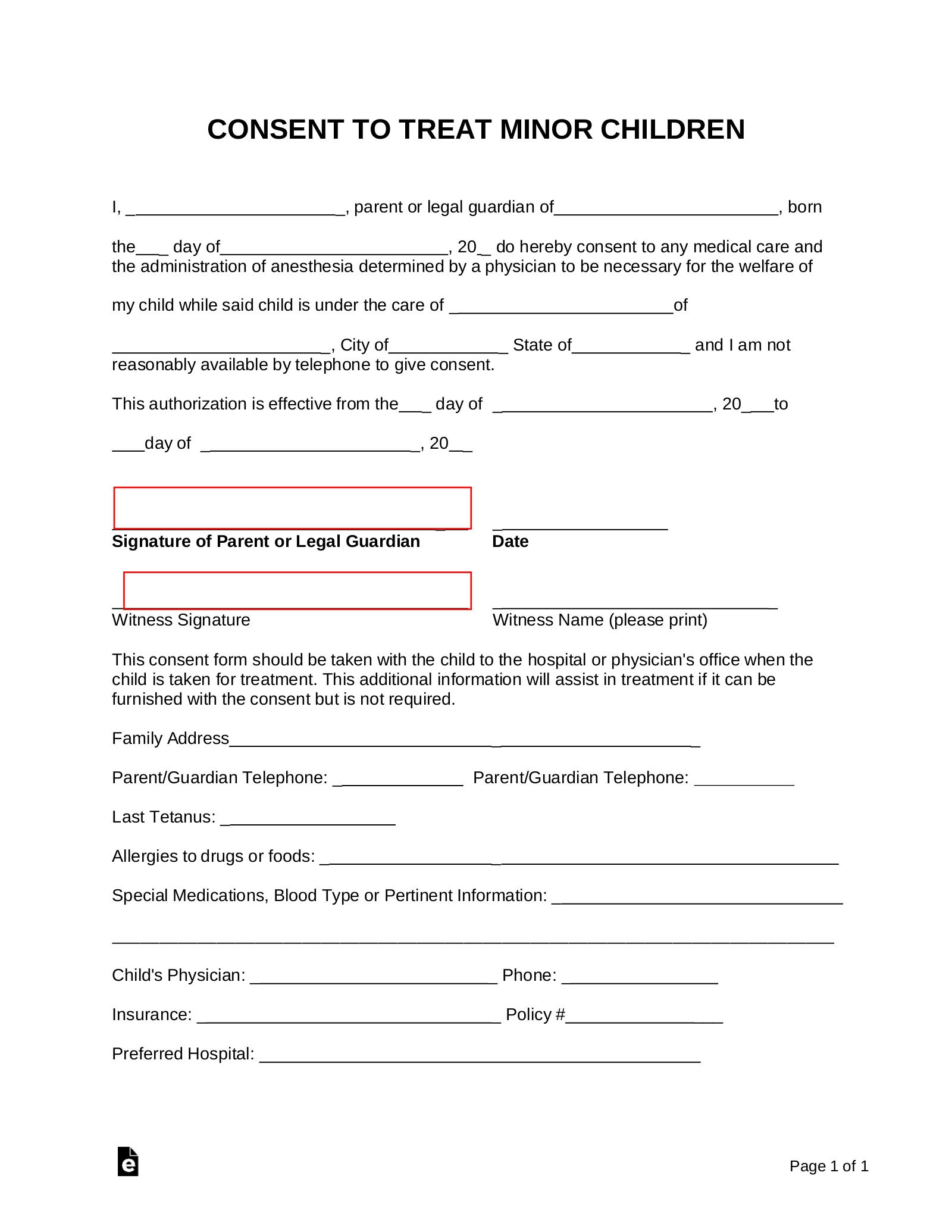
This is adequate for routine treatment such . This is no longer . Consent by a person must be in writing when required by law or by the policies of the state, territory .Patients acceptance and comprehension to written and verbal consent (PAC-VC) Patients had adequate understanding to most components of verbal assent . When you make a decision in regards to your health, you want to make sure you understand what you’re agreeing to including the .Whenever you are proposing research with human participants you must provide a form, known as an Informed Consent Form (ICF), with each proposal to indicate that the .
Informed Consent Form
Published: 24 May 2017. The College's Consent practice guideline provides an overview of the major features of the relevant legislation, pertinent definitions and the steps that nurses need to take to obtain consent. Written versus verbal consent: a qualitative study of stakeholder views of consent procedures used at the time of recruitment into a peripartum trial . In other circumstances, for example telephone interviews or some ethnographic fieldwork, this may not be possible.
Informed consent in oral health care
In some contexts verbal consent may be ethically preferable to written consent.
What does informed consent mean?
Mandatory Parental Consent to Abortion. I help take care of her and I am financially responsible for her.

As in experimental research situations, courts may impose on physicians a .verbally – for example, a person saying they're happy to have an X-ray. Nurses develop therapeutic relationships with patients and family members each day to ensure that health care concerns and .Health care situations where implied consent is not sufficient. Informed consent is a person’s decision, given voluntarily, to agree to a healthcare treatment, procedure or other intervention that is made: With adequate knowledge .30%) gave both verbal and written consent.In obtaining consent for cosmetic surgical procedures or for any type of medical or surgical work which might be regarded as less than entirely necessary to the physical health of the patient, physicians must take particular care in explaining fully the risks and anticipated results. If the service user has given you their express consent verbally, it is good practice to keep an ongoing, up-to-date record of this in .
How to obtain informed consent for research
6% of the risks of treatment.Ensuring the security, privacy, and protection of patients' healthcare data is critical for all healthcare personnel and institutions.1 Researchers must seek and obtain the informed consent of individual participants before those participants begin to be involved in research, except in the circumstances outlined in Research with Adults who Cannot Provide Informed Consent. Consent is not a simple yes/no answer in many situations.Consent to treatment is the agreement that an individual makes to receive medical treatment, care, or services, including tests and examinations. When It Is Required.person can give consent expressly (in writing or verbally) or it can be implied. Nurses have professional and legal obligations for obtaining consent.Ensuring informed consent is properly obtained is a legal, ethical and professional requirement on the part of all treating health professionals and supports person-centred care.

A lack of physical or verbal resistance (for example, where a person has a freeze response) does not indicate consent (NSW LRC 2018).Prior to administering a treatment “whether for therapeutic, preventative, diagnostic or other health-related purposes” informed consent must be obtained from the patient in accordance with O.
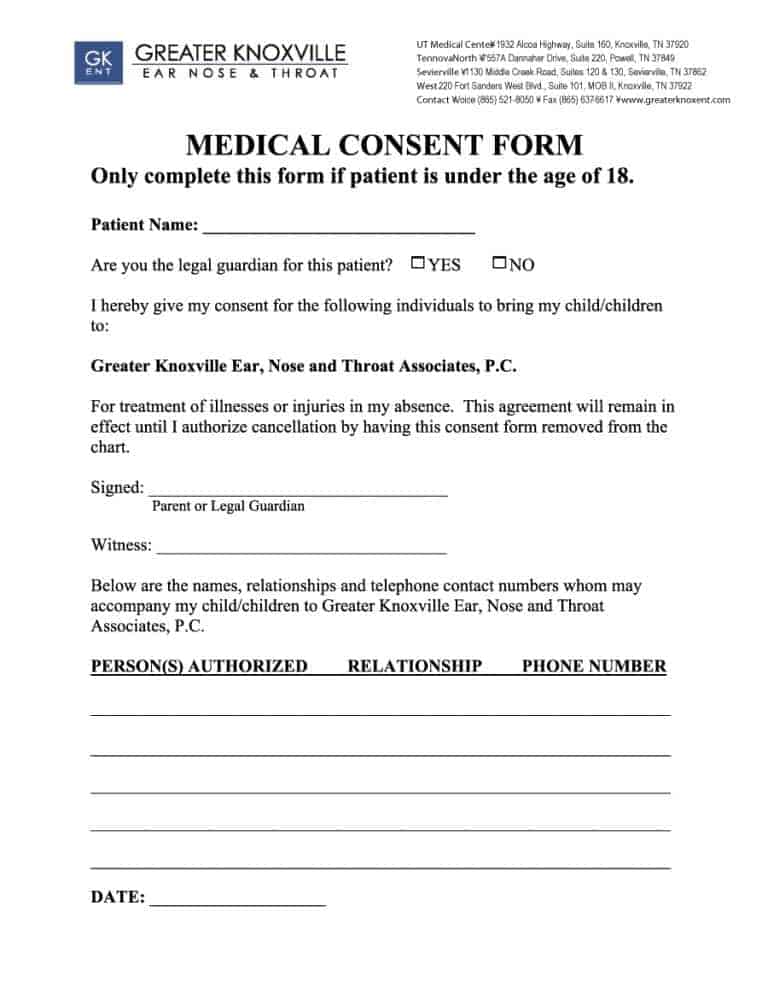
Registered nurses who do not respect this principle may be liable to both legal action by the person in their care and action by the NMC. In the past, healthcare workers often collected patient data for research and usually only omitted the patients' names.Verbal consent: A verbal consent is where a patient states their consent to a procedure verbally but does not sign any written form.17% of the benefits, and 38.Unfortunately, the emphasis on obtaining a patient’s signature as documentation of informed consent results in varying effectiveness of the communication between a clinician and a patient. The consent signature requirements from the mother and father are summarised in table 3. In many jurisdictions, unemancipated minors are not permitted to request or receive abortion services without their parents’ (or guardian’s) knowledge and consent.
Informed Consent, When It's Needed, and How It's Given
Verbal Telephone Consent In-person, face-to-face, consenting/re-consenting should always be undertaken wherever possible.
Fact Sheet for clinicians- Informed consent in health care
Evaluating nurse understanding and participation in the .