Urinary bladder surgery
If non-surgical treatments for urinary incontinence are unsuccessful or unsuitable, surgery or other procedures may be recommended. Learn how health sources are defined by the World Health Organization. Urine moves from the kidneys through narrow tubes to the bladder.
Cystectomy for Bladder Cancer
A colovesical fistula is an open connection between the colon and bladder.Surgery to remove your entire bladder is called a radical cystectomy. Bladder Cancer.Pelvic floor muscle training before prostatectomy surgery reduces post-prostatectomy incontinence, improves your quality of life, and improves pelvic floor muscle function. Is bladder incontinence . Urinary retention is when your bladder doesn’t empty when you pee.
Bladder Surgery: Purpose, Procedure, Risk & Recovery
Issues After Surgery .
Cystectomy (bladder removal)
Sling Procedures to Treat Stress IncontinenceMost surgical procedures to treat stress incontinence fall into two main categories: sling procedures and bladder neck suspension procedures. Your urinary bladder holds your urine (pee) after your kidneys clean your blood. Artificial urinary sphincter, which is when your doctor replaces your urinary sphincter with an artificial one to provide more control. The type of surgery you may need depends on which . This procedure may be recommended if the bladder has lost its support. For this purpose, a foley catheter is typically placed prior to surgery and keeps the bladder empty throughout. It is called bladder-preserving surgery because the bladder is kept in place so you can continue to urinate normally. How to Prepare. The catheter is then gently withdrawn until the cuff rests in the bladder neck.

If untreated, structural problems may lead to .Surgery for Urinary Dysfunction.Purpose of Cystectomy.Overview
Surgery for stress urinary incontinence in women
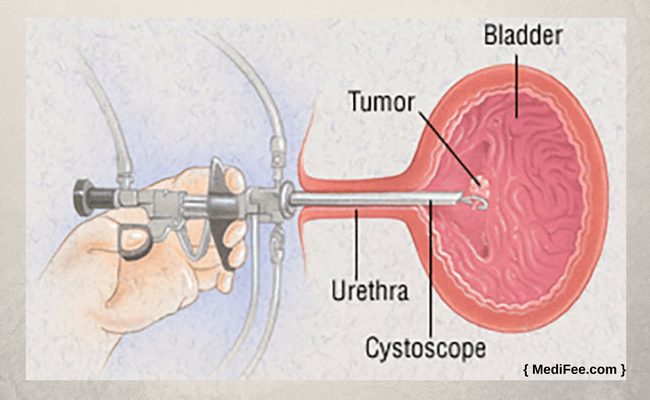
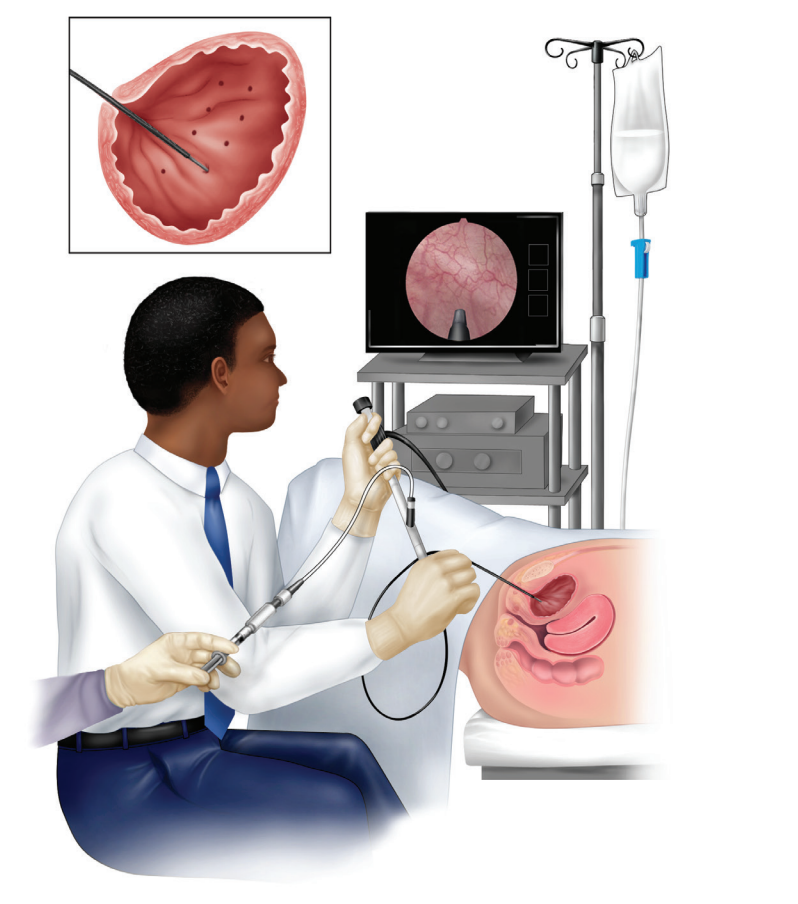
Blockages, medications or nerve issues can cause it. TURBT is a procedure to diagnose bladder cancer . Treatment may include strengthening your pelvic floor muscles or surgery.
Urinary Retention: Causes, Diagnosis & Treatment
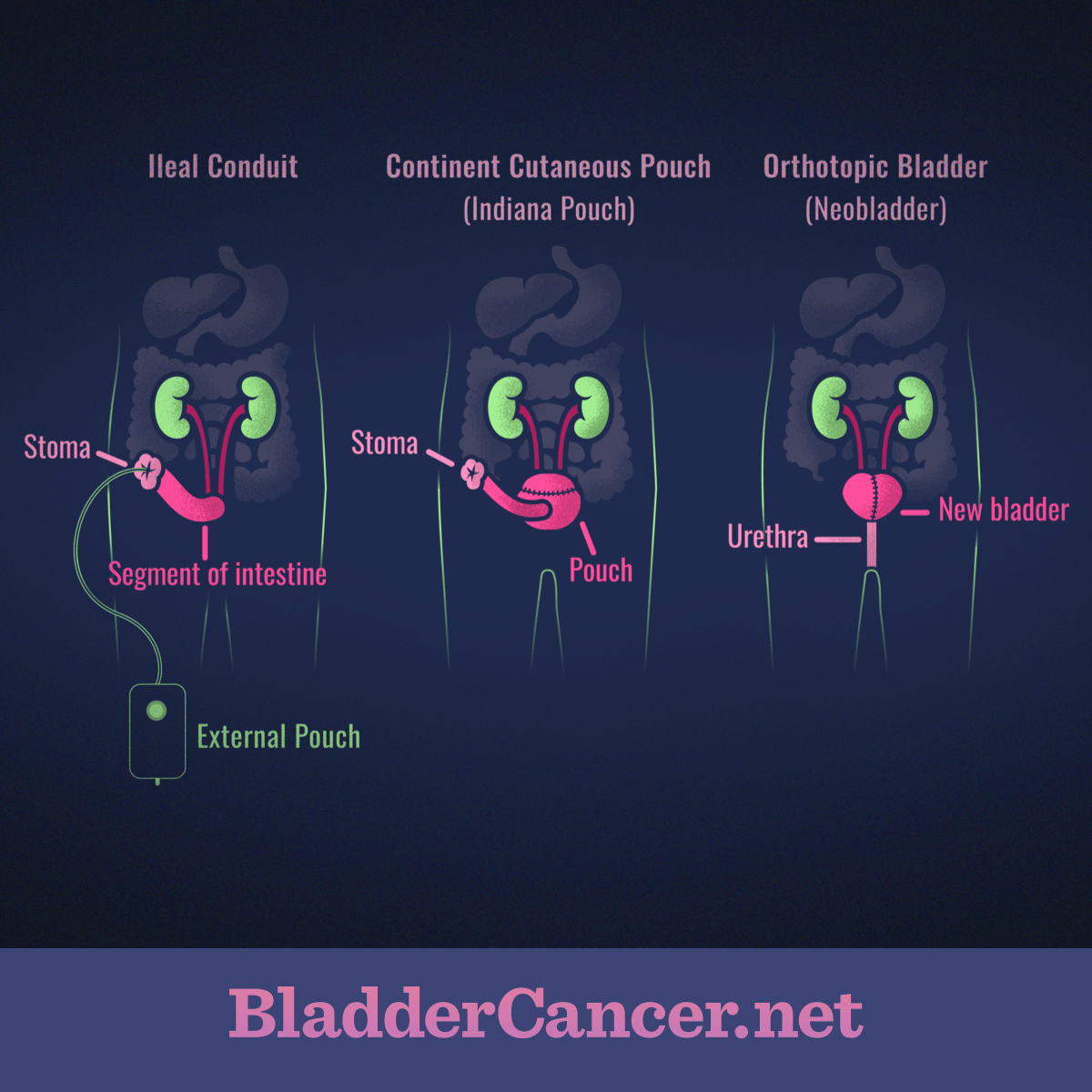
Urinary catheters may remain in place for several days or weeks while tissues heal after urinary tract surgery or treatment of urinary blockage and, in some cases, may be permanent.4K subscribers. The urinary tract begins with the kidneys and ends when urine leaves the body. The procedure takes anywhere from two to six hours. Kegel exercises can also speed up your recovery time. Before making a decision, discuss . Indiana Pouch continent urinary reservoir surgery creates an artificial bladder inside your body that you empty with a detachable catheter (long, thin tube). This surgery is the best chance for a long-term . After the surgery, you’ll press a .Bladder surgery is a procedure on your urinary bladder. The kidneys are located toward the back of the upper abdomen.Sling surgery is the most common surgery doctors use to treat urinary stress incontinence. Complex surgery to create an artificial bladder inside of the body.The typical adult human bladder will hold between 300 and 500 ml (10 .Prolapse surgery, which is more common for women.A cystocele occurs when the ligaments and muscles that hold up your bladder stretch or weaken. Like any procedure, there are risks.
When and Why a Urinary Catheter is Used
Mayo Clinic urologic surgeons have extensive experience performing cystectomy and urinary tract reconstruction for people with bladder cancer and other conditions.Nerve Stimulation to Treat Overactive BladderCertain procedures to treat overactive bladder involve stimulation — using small, electrical impulses — of the nerves that signal the need to urina. Learn about your options for surgery. Risks include urinary tract infections and bladder stretching or tearing if you don’t clean your catheters. A cystectomy is a surgical procedure that is done to remove the bladder, usually due to .

If you have stress incontinence, your doctor may recommend a procedure that helps improve control of the bladder or urethra.Surgery to remove the bladder (cystectomy) and create a urina r y diversion is a major and complicated operation. Problems, including infection, can develop and impact all of the areas of the urinary tract. It treats cancer that has spread into the muscle of the bladder wall or beyond. Urinary retention is .Changes in urination happen after surgery due to factors that impact the nervous system, such as anesthesia, medications, or pain.Overactive bladder (OAB) syndrome is a physical condition that can lead to physical and psychological symptoms. About one-third of people with overactive bladder .The bladder is a hollow organ in humans and other vertebrates that stores urine from the kidneys before disposal by urination. The aim is to cure the . A thick wall of tissue normally separates the two.A dropped bladder is when a bladder drops into the vaginal canal.

In placental mammals, urine enters the bladder via the ureters and exits via the urethra.
Cystectomy
Surgeons most often recommend it to treat bladder cancer.
Bladder Cancer Surgery: Prep, Types, Recovery
People who urinate eight or more times during the day or at least twice overnight may be diagnosed with the condition. Download Section as PDF. When empty, it lies completely within the pelvic cavity, but enlarges upward into the abdominal cavity when full.

A partial cystectomy is not commonly done for bladder cancer. This is a big operation. Two main options are available for VUR: ureteral reimplantation or . It serves as a temporary reservoir for urine produced by the kidneys.The urinary bladder is a pelvic organ that collects and holds urine before urination. Different surgical methods may be used for removing the bladder: Open surgery makes one long cut (incision) in the abdomen. Prolapsed bladder surgery is usually performed through the .The mainstay of treatment for muscle- invasive bladder cancer is surgical removal of the urinary bladder.
Bladder removal surgery (cystectomy)
The presence of the catheter facilitates identification of the urethra and bladder neck during surgery.For patients who developed PO‐UR after surgery, there was high‐certainty evidence that a hot pack or gauze soaked in warm water reduced the need for catheterization, with two patients needing this treatment to resolve one case of urinary retention. Lifestyle Adjustments.Surgery may provide a long-term solution for women with stress urinary incontinence when other treatments don't work. Elizabeth Kavaler explains more about how surgery can combat this problem. A partial cystectomy (also called segmental cystectomy) removes only part of the bladder (with the tumour). This includes a return of symptoms and difficulty emptying the bladder.Approaches to bladder cancer surgery might include: Transurethral resection of bladder tumor (TURBT).Your urinary system includes the kidneys, ureters, bladder and urethra. This is one of the main treatments for muscle-invasive or locally advanced bladder cancer . Treating Bladder Cancer.Cystoscopy, also called Cystourethroscopy, is a diagnostic procedure that allows the doctor to directly examine the urinary tract.Foley catheter is inserted through the urethra into the bladder, and the cuff is inflated. It often remains in place until the surgery is completed and you're awake and alert enough to begin urinating normally. We see this when a . Full recovery from open gallbladder surgery takes about six weeks; recovery from a laparoscopic surgery takes about four weeks. What to Expect on Day of Surgery.A cystectomy is an operation to remove the bladder. You might be in hospital for between 5 and 14 nights.
Keeping your incision site (s) clean and dry. It plays two main roles: Temporary storage of urine – the bladder is a hollow organ with distensible walls.Your urinary incontinence surgery will be performed in a hospital or surgery clinic.Suspension Procedures to Treat Stress IncontinenceA bladder neck suspension reinforces the urethra and bladder neck so that they won't sag and provides something for the urethra to compress against. Higher volumes are associated with lower complication rates. Most people recover within six weeks, but it may take up to three . It is the most anterior pelvic organ, located just behind the pubic bones . A cystostomy is a surgical procedure where a . Severe prolapsed bladders that cannot be managed with a pessary usually require surgery to correct them.
From a medical journal.Urinary reflux surgery is a procedure that stops urine from backflowing into your ureters.
Surgery for bladder cancer
Engaging your pelvic floor muscles after surgery strengthens them and improves bladder control.When the bladder is removed, urine needs to exit the body in a new way, through a urinary diversion.
Bladder Surgery
Urinary Diversion: What Is It, Types & Surgery Options
Sexually transmitted infections (STIs): Infections spread through sexual contact can also cause swelling and lead to urinary retention. You may see or feel tissue bulge through your vaginal opening or have difficulty peeing or inserting menstrual products.
Urinary Reflux Surgery: Types, Benefits, and Recovery
Restricting certain activities, like heavy lifting, swimming, or sports for one to four weeks. This may mean you need to use a urinary catheter for a period of time.
Cystectomy/Bladder Surgery: Preparation, Recovery
People with OAB experience urinary urgency and a need to urinate frequently. That’s when certain movements or actions, like coughing, sneezing, .A cystoplasty (bladder augmentation) is a surgery that makes your bladder larger so you can hold more urine.In the hands of a skilled doctor, urinary incontinence surgery is generally a safe procedure.Temps de Lecture Estimé: 8 min
Bladder Cancer Surgery
Overactive bladder is the medical term used to describe a condition in which you have a strong urge to urinate multiple times a day and overnight, even though your bladder is not full.
Cystectomy (Bladder Removal): Procedure, Risks & Recovery
A radical cystectomy removes the entire bladder. They filter waste and fluid from the blood and produce urine. 124K views 5 years ago. A cystoscopy may be recommended when a disorder of the urinary tract is suspected, including structural problems that can lead to a blockage of urine flow or a back flow of urine. The types of procedures women have vary depending on the type of incontinence surgery: Bladder augmentation surgery for overactive bladder involves an abdominal incision.
Bladder removal surgery: What you need to know
The Urinary Bladder
Partial cystectomy. Sexual intercourse may also be painful.Bladder cancer surgery ranges from minimally invasive to full removal of the bladder and restructuring of the urinary passage. The urinary system removes waste from the body through urine.Urinary incontinence and other bladder problems, like difficulty emptying the bladder or urinary hesitancy, can happen after the surgery, but they usually go away on their own.Urinary tract infection (UTI): An infection in your urinary tract can cause your urethra to swell or cause weakness in your bladder, both of which can cause urinary retention. Taking your pain medication as directed. Written by WebMD Editorial Contributors.Indiana Pouch Surgery.
Bladder Augmentation (Cystoplasty): Procedure & Recovery
Assists in the expulsion of urine – the musculature of the .Surgery to remove the bladder (cystectomy) A cystectomy is an operation to remove your bladder.

If you are considering surgery, be sure to find a board-certified surgeon . There are many different types of bladder surgery. Some surgeons have advocated combined repair of the exstrophy and epispadias defect as the initial management, closing the bladder and repairing the epispadias in one procedure.What Is Bladder Prolapse Surgery? Medically Reviewed by Jabeen Begum, MD on October 10, 2023. A midline, caudal abdominal approach is made. It is important to have this surgery in a specialised centre with a surgeon who does a lot of cystectomies. [ show] Surgery is part of the treatment for most .